Researchers at Montefiore Einstein Cancer Center (MECC) discovered that many cases of Acute Radiation Dermatitis (ARD) involve a common skin bacterium and that a simple, low-cost treatment can prevent sever cases. Their findings were reported in two papers published in JAMA Oncology.
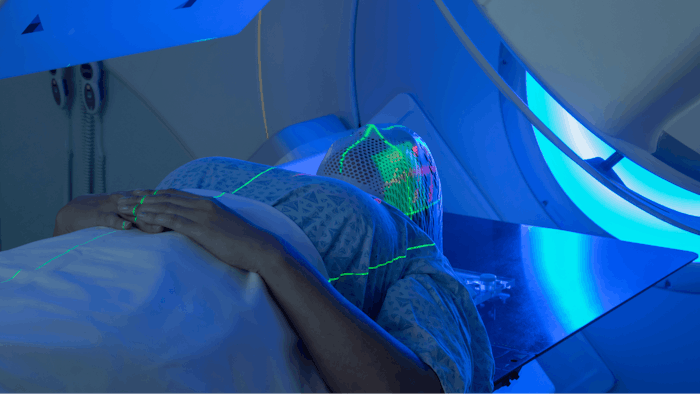
Acute radiation dermatitis (ARD) affects up to 95% of people undergoing radiation treatment for cancer. Sever cases can cause significant swelling and skin ulcers that can affect quality of life, yet there is not much known about why this condition occurs and no standardized treatments for preventing sever ARD have been widely adapted.
"Until now, ARD was assumed to result simply from the skin being burned by the radiation, which meant that not much could be done to prevent it," said Beth N. McLellan, M.D. Director or Supportive Oncodermatology at Montefiore Einstein Cancer Center, Chief of the division of dermatology at Montefiore Health System and Albert Einstein College of Medicine, and senior author of the two studies. "The readily available treatment we've developed and clinically tested could potentially save hundreds of thousands of people each year in the U.S. from severe ARD and its excruciating side effects."
Identifying the Cause
Staphylococcus aureus (SA) bacteria, often shortened to "staph," typically live harmlessly on the skin, often in the nose and armpits. Radiation weakens the skin's structure at the treatment site and can result in infection by allowing SA to break through the skin's outer layer. Courses of radiation therapy—routinely requiring daily treatments over several weeks—increase the risk for skin infection to occur.
In one of the JAMA Oncology studies, the MECC researchers enrolled 76 patients undergoing radiation therapy for cancer. Bacterial cultures were collected from patients before and after radiation treatment, from three different body sites: inside the nose, from skin in the radiated area, and from skin on the side of the body not exposed to radiation.
Related: Alphyn Biologics' AB-101 Atopic Dermatitis Treatment Shows Promise in Ongoing Phase 2a Trial
Before treatment, about 20% of patients tested positive for SA, but did not have an active infection. Following treatment, 48% of those patients who developed severe ARD tested positive for the presence of SA, compared with only 17% of patients who developed the mildest form of the condition.
"This study clearly showed that SA plays a major role in ARD," said Dr. McLellan. "The good news is we have a lot of tools to fight these bacteria. In a second study, we tested a topical antibacterial drug combination we thought would be effective and easy for people to use."
Severe ARD Prevention
The second study enrolled 77 patients undergoing radiation therapy, all but two of whom had breast cancer. Participants were randomized to receive either the standard of care at MECC (normal hygiene and moisturizing treatment such as Aquaphor), or the experimental antibacterial regimen. This treatment involved using the body cleanser chlorhexidine along with mupirocin 2% nasal ointment twice a day for five days, every other week, throughout their radiation treatment.
Although more than half the patients treated with the antibacterial regimen developed mild-to-moderate ARD, no patients developed moist desquamation, the most severe type of ARD that causes the skin to break down and develop sores, and no patients experienced adverse effects from the treatment. In contrast, severe ARD affected 23% of participants receiving the standard of care.
The papers are titled "Association of Staphylococcus aureus Colonization With Severity of Acute Radiation Dermatitis in Patients With Breast or Head and Neck Cancer" and "Bacterial decolonization for prevention of radiation dermatitis: a randomized clinical trial." Co-authors on both papers include: Yana Kost, B.A., Alana Deutsch, M.D., Nitin Ohri, M.D., M.S., H. Dean Hosgood, Ph.D., Johanna P. Daily, M.D., M.S. and Kosaku Shinoda, Ph.D. Additionally, Alexandra K. Rzepecki, M.D., and Mathew R. Birnbaum contributed to the S. aureus paper. Karolina Mieczkowska, M.D., Roya Nazarian, Ahava Muskat, B.S., Juan Lin, Ph.D., and Rafi Kabaritti, M.D., also contributed to the bacterial decolonization paper.











